Assessments

Assessments you may see or hear about while your loved one is recovering from a brain injury
Understanding the various assessments conducted during the rehabilitation process can provide valuable insight into your loved one's journey to recovery after a brain injury. These assessments help healthcare professionals evaluate their cognitive, physical, emotional, and functional abilities, guiding personalized treatment plans and monitoring progress over time.
Neurological Examination
A comprehensive neurological examination is performed to assess cranial nerves, motor strength, coordination, reflexes, sensation, and other neurological functions. This evaluation helps determine the extent and nature of the brain injury.
Cognitive Assessments
Cognitive assessments evaluate memory, attention, executive function, language skills, visuospatial abilities, and problem-solving.
Functional Assessments
Functional assessments measure the individual's ability to perform activities of daily living (ADLs) independently, including dressing, grooming, bathing, feeding, mobility, and household activities.
Psychological and Emotional Assessments
These assessments evaluate emotional well-being, coping skills, mood disorders (such as depression and anxiety), and adjustment to the brain injury.
Speech and Language Assessments
Speech and language assessments help evaluate language deficits and guide interventions for individuals with aphasia, swallowing, and cognitive difficulties.
Physical Assessments
Physical assessments focus on the individual's physical abilities, including balance, coordination, strength, range of motion, and endurance. These evaluations inform physical therapy interventions.
Occupational Therapy Assessments
Occupational therapists assess vocational skills, hand function, and cognitive abilities related to daily tasks.
Vision and Perception Assessments
Assessments like the Functional Vision Assessment and the Rivermead Perceptual Assessment Battery evaluate visual deficits and perceptual impairments resulting from the brain injury.
Social and Community Integration Assessments
These assessments focus on social skills, relationships, and the ability to reintegrate into the community, providing valuable information for rehabilitation planning.
Pain Assessments
Assessments help understand the nature and severity of pain experienced by individuals with brain injuries, guiding appropriate pain management strategies.
Each assessment plays a crucial role in tailoring care plans to meet the unique needs of individuals with brain injuries and supporting their journey towards recovery. If you have specific questions about assessments, do not hesitate to ask the doctor’s and rehab team!
The most common assessments you may hear or see are…
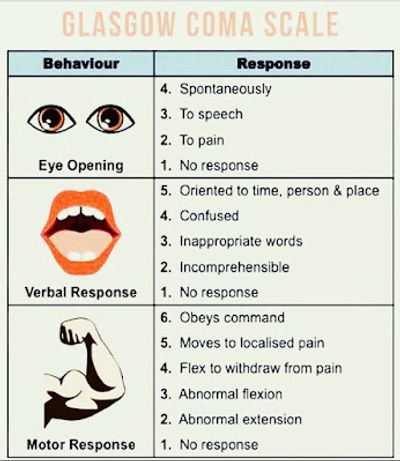
The Glasgow Coma Scale (GCS)
The Glasgow Coma Scale (GCS) is like a quick test doctors use to see how awake and aware someone is after an injury or illness affecting the brain. It helps them understand how severe the problem might be and track changes over time.
Here's how it works:
- Eye Opening: Doctors check if the person opens their eyes on their own or in response to someone talking to them, or if they only open their eyes when they're poked or pinched. Each way the person opens their eyes gets a different score, with opening on their own getting the highest score.
- Verbal Response: Doctors see how the person responds when they talk to them. They note if the person can answer questions correctly and make sense, or if they're confused, say strange things, make sounds without meaning, or don't respond at all.
- Motor Response: Doctors test how the person moves or reacts when touched or when they're in pain. They check if the person can follow simple commands like squeezing a hand or moving a body part in response to pain. The way the person moves or reacts determines their score.
Each of these three parts gets a score, and then those scores are added up to get a total score. The highest possible score is 15, which means the person is fully awake, aware, and responsive. The lowest score is 3, which means the person is in a deep coma and not responding at all.
Doctors use the total score to understand how serious the brain injury or condition might be and to decide on the best treatment. They may also use it to track the person's progress over time.
The Rancho Los Amigos Scale (RLAS)
The Rancho Los Amigos Scale (RLAS) is like a tool that helps doctors and therapists understand how a person is recovering after they've had a brain injury, like a concussion or a more serious injury. It helps them figure out what stage the person is at in their recovery and what kind of help they might need.
The scale has eight levels, kind of like steps, and each level describes how a person might act or respond as they recover. Here's a simple explanation of each level:
- Level I: No Response: The person is in a deep coma and doesn't react to anything around them.
- Level II: Generalized Response: The person might make some movements, like pulling away from pain, but they're not really responding in a meaningful way.
- Level III: Localized Response: The person starts to react more to what's happening around them. They might respond to pain or try to follow simple commands, but it's still inconsistent.
- Level IV: Confused-Agitated: The person becomes really restless and might even get upset or aggressive, but they're still pretty confused and not really aware of what's going on.
- Level V: Confused-Inappropriate: The person might calm down a bit, but they're still confused and might say or do things that don't make sense.
- Level VI: Confused-Appropriate: The person starts to understand things a bit better and might follow simple instructions, but they still need help with a lot of things.
- Level VII: Automatic-Appropriate: The person starts to do things more automatically, like eating or getting dressed, but they might still need reminders or help.
- Level VIII: Purposeful-Appropriate: The person is much more aware and can do most things on their own. They might still have some problems, but they're able to live pretty independently.
Doctors and therapists use this scale to see where someone is in their recovery and to plan the best way to help them get better. It helps them understand what the person can and can't do and what they need help with.


The JFK Coma Recovery Scale
The JFK Coma Recovery Scale (CRS) is like a test that helps doctors and therapists understand how much a person is waking up and responding after being in a coma or a very deep state of unconsciousness. It's used to assess someone's progress and see how their brain is recovering.
Here's a simple breakdown of how the CRS works:
1. Observation: Doctors and therapists watch the person closely to see if they're showing any signs of waking up or responding to things around them.
2. Stimuli: They might try different things to see if the person reacts, like calling their name, shining a light in their eyes, or touching them gently.
3. Responses: Based on how the person reacts, they're given a score on different parts of the scale. These scores help track their progress and give a better idea of how aware and responsive they are.
4. Categories: The CRS looks at things like eye movements, communication, and motor responses (like moving arms or legs). Each category has different levels, from no response at all to more purposeful movements and interactions.
5. Assessment: By combining all the scores, doctors and therapists can get an overall picture of how much the person is waking up and responding. This helps them plan the best care and therapy for the person's recovery.
Overall, the JFK Coma Recovery Scale is a way for healthcare providers to understand and track someone's progress as they come out of a coma or deep unconsciousness. It helps them make decisions about treatment and support to help the person recover as much as possible.

Another common assessment you may see or hear about is a “swallow test” which is…
A videofluoroscopic swallow study is like a special X-ray test that helps doctors and speech therapists see how well someone can swallow food and liquid. It's used when someone has trouble swallowing, which can happen after a stroke, injury, or other medical issues.
Here's how it works in simple terms:
1. Preparation: The person sits or stands in front of a machine that takes X-ray pictures called fluoroscopy. It's like a big camera that can see inside the body.
2. Testing: The person eats or drinks foods and liquids mixed with a special kind of dye called barium. Barium shows up really well on X-rays, so doctors can see it moving through the throat and into the stomach.
3. X-ray Pictures: While the person eats or drinks, the fluoroscopy machine takes lots of pictures in real-time. These pictures show exactly what's happening inside the person's throat as they swallow.
4. Observation: Doctors and speech therapists watch the X-ray pictures closely to see how well the person swallows. They look for any problems, like food going into the lungs instead of the stomach or if the food is getting stuck in the throat.
5. Analysis: Based on what they see, the doctors and therapists can figure out if there are any issues with the person's swallowing and what might be causing them.
6. Recommendations: After the test, the doctors and therapists can suggest ways to help the person swallow better. This might include changes to their diet, special exercises, or techniques to make swallowing easier and safer.
Overall, the videofluoroscopic swallow study is an important test that helps healthcare providers understand and improve a person's ability to swallow safely and comfortably.
Copyright © 2024 Brain Care Networks - All Rights Reserved.
Powered by GoDaddy
This website uses cookies.
We use cookies to analyze website traffic and optimize your website experience. By accepting our use of cookies, your data will be aggregated with all other user data.